FOREWORD
I write this amidst the global reckoning that 3.3 billion people who are least responsible for total emissions are bearing the greatest health impacts from climate change. We need a transformation of health systems to better prevent, predict, detect, and respond to disease outbreaks caused or worsened by climate change.
Against this backdrop, Self Testing is an increasingly valuable tool to assess personal health status, especially in the most marginalized communities that lack access to health systems. The introduction of Self Testing shifts the agency of personal health care to the hands of the people, while simultaneously reducing health system burden and strengthening community health systems.
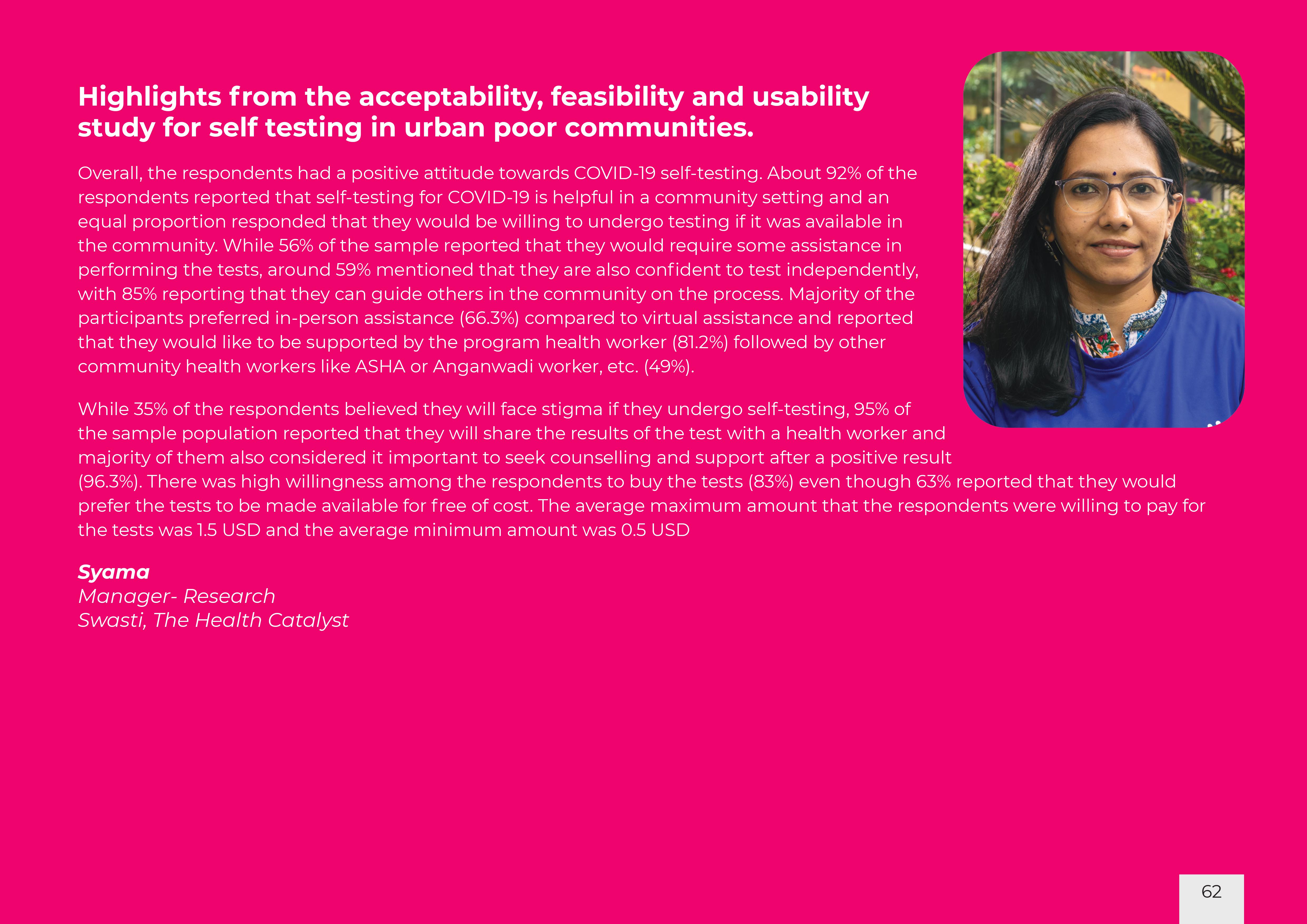
During the COVID-19 pandemic, it was critical that Self Testing as a preventive measure was adapted in a widespread manner and not limited to a few. We, therefore set out to understand the usability, feasibility and affordability with regards to uptake of Self Testing.
Our learnings were manifold, and we are confident that Self Testing can be introduced successfully into communities with peer assistance. This journey has also shown us that when communities are armed with their own health information, they have the tools and confidence to not only tackle myths and misconceptions in their own groups, but also overcome hesitancy. The ability to conduct Self Testing in the privacy of their own space also increased comfort levels with and sustainable use of the approach.
This playbook is a result of an Action Research project undertaken by Swasti, The Health Catalyst - a public health non profit headquartered in Bengaluru, India with support from The Rockefeller Foundation. The playbook breaks down the “how to” along with relevant forms, formats and documentation, offers information and insights including community voices and stands in as a toolkit and resource guide for the introduction of self testing in community settings.
As we collectively gear up to protect the most marginalized from the greatest health impacts from climate change - including possible future pandemics – we hope this playbook will help in setting up the required systems - towards community systems strengthening for health systems strengthening.
Deepali Khanna
Vice President
Asia Regional Office, The Rockefeller Foundation