
What is a playbook?
A playbook includes "process workflows, standard operating
procedures, and cultural values that shape a consistant
response-the play." it borrows from some of the aristotelian
elements of the play -
Plot - The arrangement of events or incidents on the stage. The plot is composed of "clearly defined problems for characters to solve."
Character - The agents of the plot. the people
Theme - The reason for the play. The purpose
3 of the 6 Aristotelian elements of the play
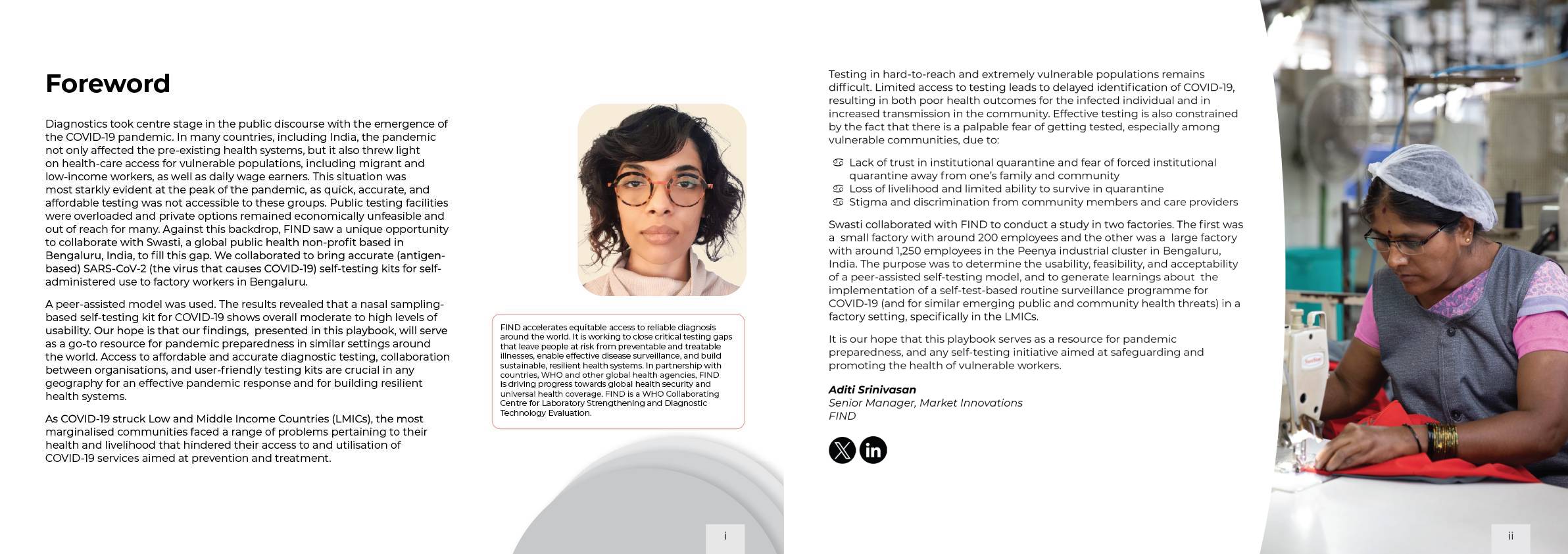
Foreword
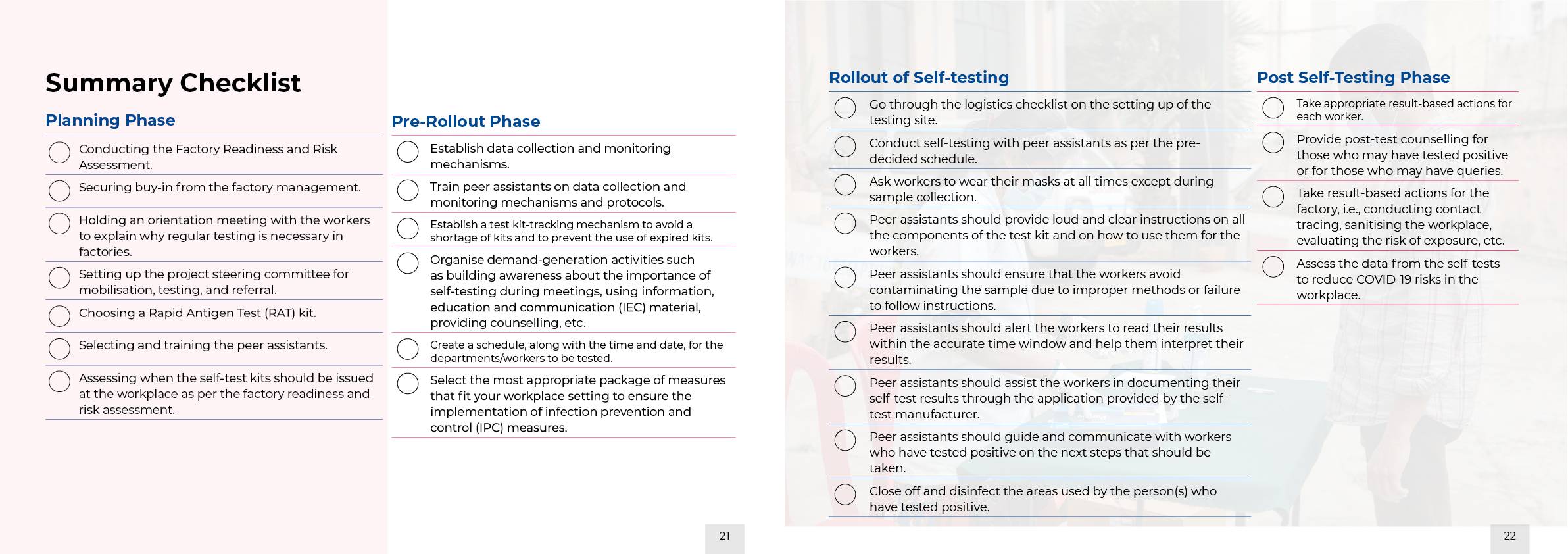
Summary Checklist

This playbook, Self-Testing in Factories | India: A Playbook for Global Pandemic Preparedness, has been designed to be used in the field by practitioners
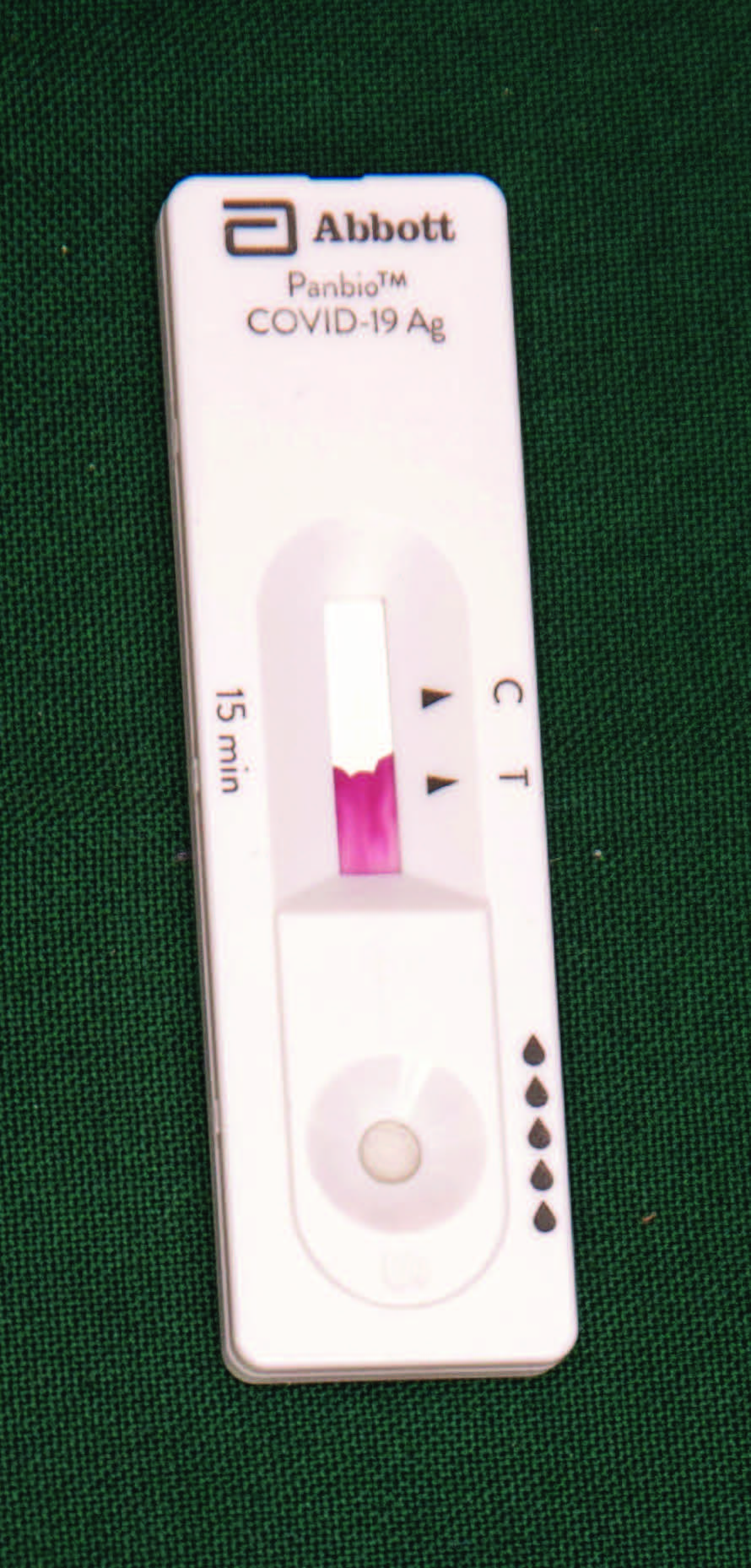
You can use the playbook to adopt self-testing measures and guidance not only for COVID-19 but also for any self-test in the future in terms of global pandemic preparedness. The sections can be adapted for any workplace setting such as offices, shops, and other establishments. Given the nature of the activities, the approach is also applicable across geographies and industries.
The logical layout of the playbook, and therefore its independent use in different settings, conditions, and circumstances, is based on the following:
The Why? - Understanding the logic of selftesting and its merits, especially in the context of worker safety, access of workers and their communities to have knowledge about their own health, and an individual’s agency in terms of securing one’s health care. This can be used for advocacy for self-testing in factories. You will find this on pages 3-4 in the chapters Plot: Problem Statement and Purpose and Objective.
The Who? – Recognizing the roles that various people need to play. These could be existing personnel who take up various roles to make self-testing at the workplace a stress-free and smooth process. This can be used to understand the role of the human resource personnel who will need to be ideally deployed. You will find this on pages 6-10 in the chapter People.
The Key Differentiator – Gaining insight into peer-assisted self-testing. The key success factor and differentiator in making the self-testing method work and why it works. This can be used to adapt this approach to different situations. You will find this on page 11 in the chapter The Secret to Success: Peer-Assisted Self-Testing.
Where? – Choosing the right places and addressing concerns about privacy in any health activity setting — whether it should be stand-alone or integrated — is a powerful and valid concern. This helps in understanding the importance of physical space. This can be used to physically alter places or to book suitable places required for self-testing. You will find this on pages 15–18 in the chapter Places.
The When? – Rolling out self-testing successfully in any setting always rests on two axes: Axis 1 – The health-seeking behaviour of an individual; and Axis 2 – The environment that dictates the urgency of self-testing or that enables selftesting. It is also important to take into account the scale at which self-testing is planned to be rolled out. This is a crucial insight that helps reduce panic or stress in any individual, demographic group, or community. This can be used as a rubric or framework to make decisions pertaining to self-testing. You will find this on pages 22–29 in the chapter Act 1. Scene 1. The Planning Phase.
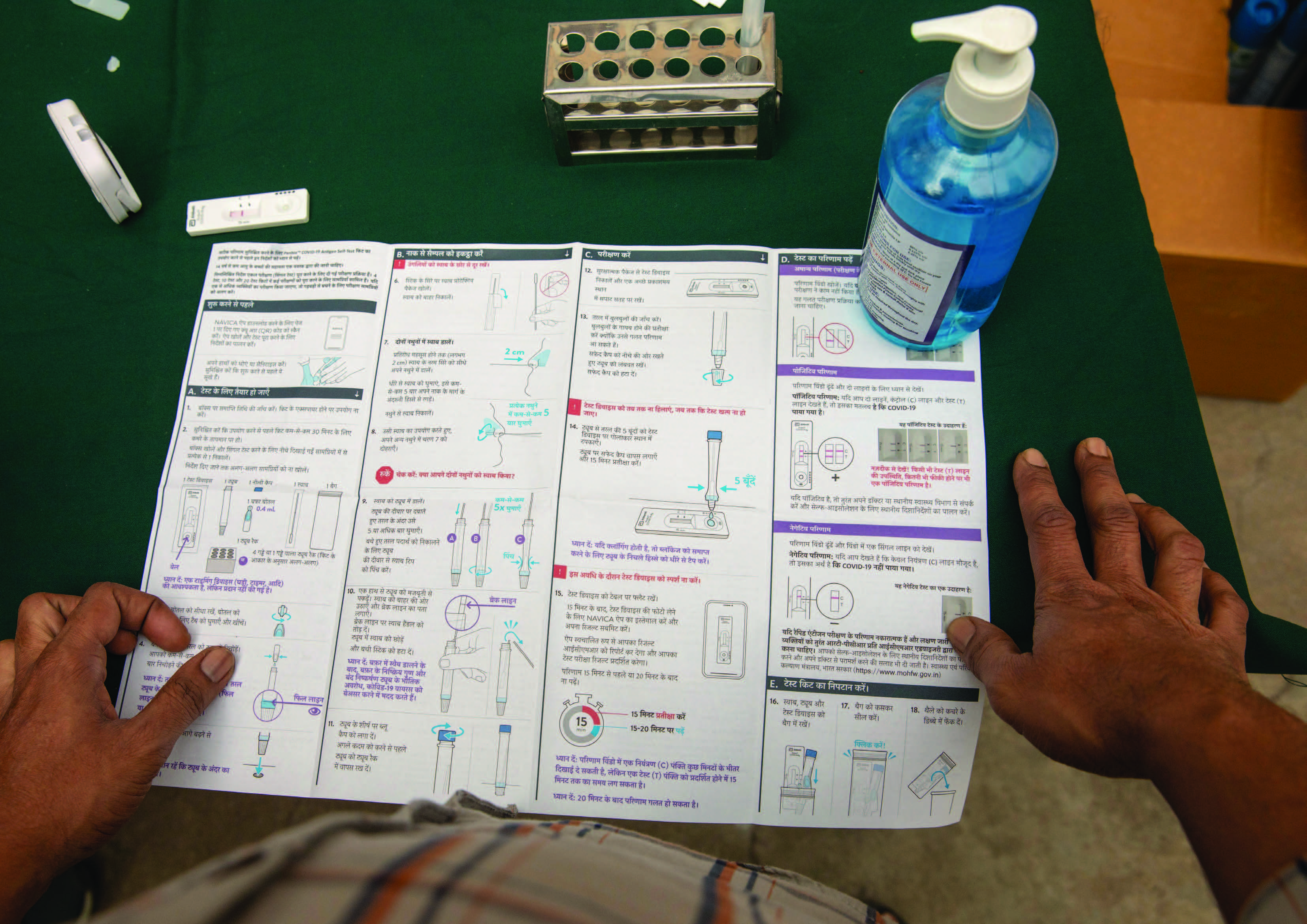
The How? – While the entire playbook is essentially about “The How?”, the logical layout of the sections is, in essence, “The How”. This can be used to design self-testing campaigns and events, or to keep these campaigns and events rolling throughout the year in order to reach out to a specific group of the most vulnerable people or to take a census approach. You will find this on pages 32–67 in the chapters Act 1. Scene 1. The Planning Phase; Act 1. Scene 2. The Pre-Rollout Phase; Act 2: The Rollout of the Self-Testing Phase; and Act 3: Post the Self-Testing Phase and Stage Directions.
Hence, depending on which question you are seeking an answer to in the context of self-testing in the workplace, the playbook is designed to help you as a whole or in parts.
No One is safe till EveryOne is safe
As the COVID-19 lockdowns eased and as workplaces started opening up, worker safety and the early identification of potential outbreaks became important requirements for keeping communities safe. Many industries and sectors that provide essential services such as banking and manufacturing struggled to stabilize themselves due to large numbers of their staff getting repeatedly infected. Gradually, the major industry players, based on epidemiologic indications, realized that COVID-19 was here to stay, and that they needed to prepare the economy and, more importantly the workers, to remain resilient in the face of imminent waves of infection. The two key ways of tackling this issue were to (a) increase the rates of vaccination; and (b) institute policies for regular screening and periodic COVID-19 testing at workplaces. These measures were important for recovery not only to ensure business continuity but also to protect employee well-being and health at all times.
Settings where workers are in close proximity, such as manufacturing units and garment factories, are at particularly high risk of large outbreaks. Typically, these workplaces exist in industrial clusters or informal settlements, and outbreaks in these units can lead directly to outbreaks in surrounding communities, and vice versa. Workers usually hail from marginalised communities such as migrants, daily wage earners, and the urban and rural poor who generally have lower level of access to health systems and health information and who often skip health check-ups entirely to avoid compromising the earning of their daily wage.
The information on self-testing in this Playbook offers guidance to help factory owners, workplace managers, and policy makers explore suitable options for selftesting for vulnerable populations, gather insights into what works and what does not, and deploy communication strategies to address myths and misconceptions. The playbook outlines the steps required for incorporating self-testing activities that can be undertaken for smooth planning and for rolling out the self-testing measures at the workplace.
In the playbook you will find:
The playbook divides the entire process into 3 Acts, which are as follows:



What does the Testing Supervisor need?
Who can be the Testing Supervisor in your workplace?




Who are they: Doctors, nursing staff, or employee responsible for worker welfare
What does the Clinical Team need to know?
If the clinical team members / trained welfare officers are not used to working or interacting with vulnerable populations, it is important to have sensitization sessions on the importance of providing respectful care. At the outset, it is important for the clinical team members / trained welfare officers to discard any assumptions they may have about the information on diseases and health care known or available to workers, or their ability to find this information by themselves. Migrant and daily wage workers may have had negative experiences and hence clinical team members / trained welfare officers should be briefed about answering specific health-related questions respectfully, sensitively, and carefully. During the COVID-19 pandemic, many people did not have access to general health care, even when they needed it most. So if testing initiatives for vulnerable populations are implemented during a pandemic, clinical teams should also use these occasions to address the general clinical concerns of workers and other vulnerable populations.
In this context, it is imperative for the clinical team member / trained welfare officer to carry out the following functions:
| 1. | Provide pre- and post-counselling on what the self-test entails and what to expect. |
|---|---|
| 2. | Actively assist the workers in conducting the self-test |
| 3. | Ask workers if they have any questions or concerns and respectfully answer or address their questions or concerns, no matter how basic they may seem. |
| 4. | Help workers read the test results and address their concerns about treatment and facing stigma or discrimination if they test positive while deploying the protocol on positive test results. |
| 5. | Request workers to repeat the self-test the next day if they test negative and if they are experiencing or exhibiting symptoms. |
| 6. | Explain the importance of attending routine testing programmes when those who test negative are selected for random testing. |
Who are they: Unit supervisors or mid-level managers in the factory
What do Non-Clinical Personnel need?

Situationally aware management: Anticipate interference and disturbances and have factory management informed and at hand who can handle issues as they come up.
In partnership with the peers, choose a location for peer-assisted self-testing that is most convenient and safest for them. Identify a location to conduct testing in the factory or workplace. This could be a room or a temporary setup at the workplace, such as a kiosk. The following are some examples of places where you can conduct testing for your workers:
If there are multiple sites or locations in the same workplace, it is important to ensure that all the sites and locations meet the following criteria.
The testing location should be: